Attention-deficit/hyperactivity disorder (ADHD) is one of the most commonly diagnosed neurodevelopmental conditions today, often recognized by symptoms such as inattention, impulsivity, and hyperactivity. But what if some ADHD diagnoses are actually something else—something rooted in trauma?
Dissociative disorders, particularly those linked to childhood trauma, can manifest in ways that mimic ADHD, leading to frequent misdiagnosis. This overlap raises an important question: Could what looks like ADHD actually be a form of dissociation?
The Symptom Overlap: ADHD vs. Dissociation
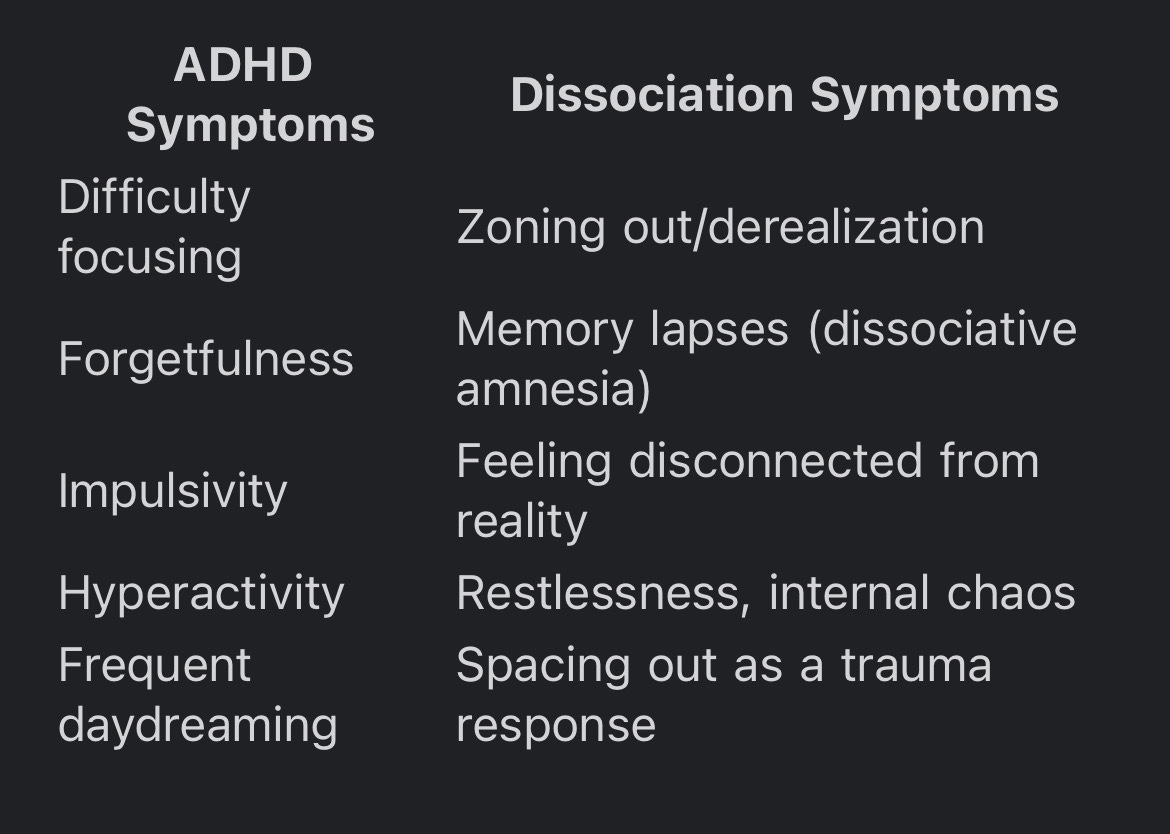
At first glance, ADHD and dissociation seem like entirely different experiences—one is typically seen as a brain-based executive functioning disorder, while the other is a response to overwhelming trauma. However, the symptoms often look strikingly similar:
Both ADHD and dissociation involve difficulties with attention, memory, and self-regulation. However, the root causes are different: ADHD is a neurodevelopmental condition present from birth, while dissociation is often a defense mechanism triggered by traumatic experiences.
Why Dissociation Can Be Mistaken for ADHD
Zoning Out vs. Inattention
People with ADHD often struggle to sustain attention due to a lack of dopamine regulation.
People with dissociation may "check out" as an involuntary response to stress or triggers, making it look like inattention.
Forgetfulness vs. Dissociative Amnesia
ADHD-related forgetfulness is often due to working memory deficits.
Dissociation can cause memory gaps, where entire experiences are blocked out, sometimes without the person realizing it.
Hyperactivity vs. Trauma-Induced Restlessness
ADHD hyperactivity is linked to an underactive dopamine system, making movement a way to stimulate focus.
Restlessness in trauma survivors often comes from hypervigilance—constantly scanning for danger.
Impulsivity vs. Emotional Dysregulation
ADHD impulsivity happens because of difficulty with impulse control.
People with dissociative disorders may act impulsively when emotionally triggered, especially if different dissociated states take control at different times.
Why the Misdiagnosis Matters
Misdiagnosing dissociation as ADHD can lead to ineffective treatment. Stimulant medications, commonly prescribed for ADHD, do not address dissociation and may even worsen symptoms in trauma survivors. A trauma-informed approach—including therapy modalities like EMDR (Eye Movement Desensitization and Reprocessing) or parts work (such as Internal Family Systems, IFS)—may be more effective for someone with dissociative symptoms.
Additionally, individuals with unrecognized dissociation may feel like they are failing at ADHD treatment when, in reality, their brain is using a different coping mechanism altogether.
How to Tell the Difference
If you or someone you know has an ADHD diagnosis but feels like something deeper is going on, consider these questions:
Do you experience memory gaps that feel larger than typical forgetfulness?
Do you feel disconnected from yourself or reality?
Have you experienced significant trauma, especially in childhood?
Do your attention problems get worse in stressful situations?
If the answers suggest dissociation, it may be helpful to seek an evaluation from a therapist trained in trauma and dissociation, rather than just ADHD.
Final Thoughts: Looking Beyond ADHD
While ADHD is a very real and valid condition, it’s important to recognize when symptoms might point to something else—especially dissociation. Given the strong link between trauma and attention issues, ensuring an accurate diagnosis can make all the difference in getting the right support.
If you suspect your ADHD diagnosis might not tell the full story, consider exploring trauma-informed care. Healing from dissociation isn’t about improving focus—it’s about reconnecting with yourself.
EMDR can be an incredibly powerful healing modality for trauma. If you’re ready to start your healing journey, reach out to me at PhiladelphiaEMDR.com